Venereal granuloma: diagnosis, features, and treatment methods
- Description of Venereal Granuloma
- Etiology of Venereal Granuloma
- Clinical picture of Granuloma inguinale
- Expert opinion on the treatment of Granuloma inguinale
- Diagnosis of Venereal Granuloma
- Treatment of Venereal Granuloma
- Prevention of Venereal Granuloma
- Interesting aspects of Venereal granuloma
- FAQ
Description of Venereal Granuloma
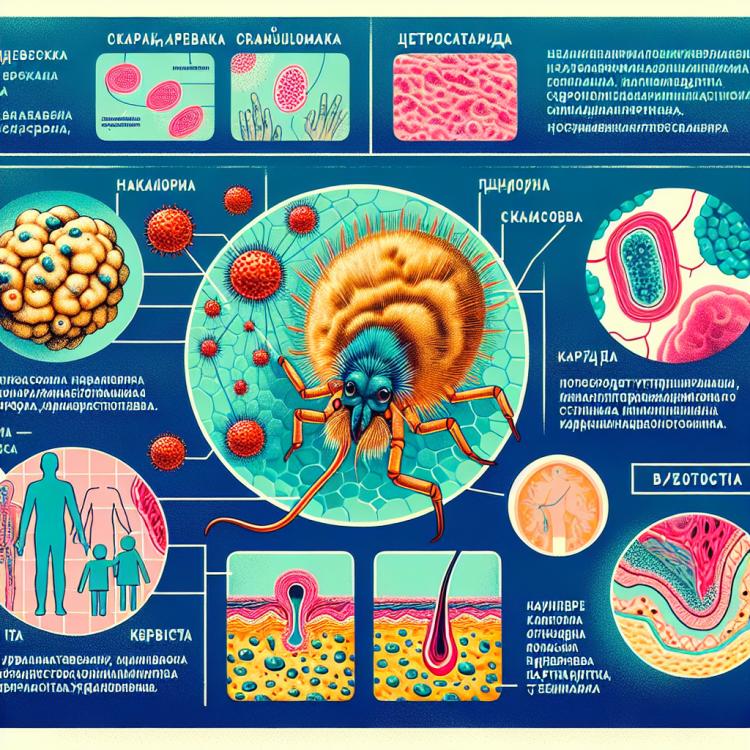
Venereal granuloma, also known as inguinal granuloma, is a chronic infectious disease caused by a bacterium called Calymmatobacterium granulomatis. The disease is characterized by the formation of painful ulcers on the skin and mucous membranes, most commonly in the genital area, around the anus, or in the mouth.
In venereal granuloma, there is a decreased immune response of the body, which contributes to the development of the infection. Characteristic signs of the disease include ulcers with a granulation base, polypoid formations, and abundant discharge. Diagnosis often requires a biopsy of the formations and microscopic examination. Treatment is based on the use of antibiotics, such as doxycycline or erythromycin, in combination with appropriate local measures.
Etiology of Venereal Granuloma
Venereal granuloma is caused by the bacterium Calymmatobacterium granulomatis, which enters the skin or mucous membrane through microtraumas or contact with infected tissues under the influence of risk factors such as improper hygiene behavior, low socio-economic status, and environmental exposure. The disease is prevalent in countries with hot and humid climates, as well as with high population density, which contributes to the formation of endemic foci of infection. The spread of venereal granuloma usually occurs through sexual transmission; however, contact and household infection is also possible with direct contact with infected tissues.
- Calymmatobacterium granulomatis bacterium: the main cause of Granuloma inguinale is an infection caused by this bacterium, which penetrates the skin or mucous membrane through microtraumas.
- Risk factors: improper hygiene practices, low socio-economic status, and environmental exposure increase the likelihood of contracting Granuloma inguinale.
- Distribution of the bacterium: the disease is more commonly found in countries with hot and humid climates, as well as high population density, which promotes the formation of endemic infection foci.
- Mode of transmission: Granuloma inguinale is usually transmitted sexually; however, there is also the possibility of contact-household infection through direct contact with infected tissues.
- Infected tissues: the bacterium penetrates through microtraumas in the skin or mucous membrane, which increases the likelihood of developing Granuloma inguinale.
Clinical picture of Granuloma inguinale
The clinical picture of Granuloma inguinale is characterized by the appearance of painful ulcerative lesions on the skin or mucous membranes in areas of contact with infected tissues. The ulcers often have a granulation base, are surrounded by an inflammatory edge, and may bleed upon trauma. Patients may experience localized pain, itching, and discomfort, which leads to a deterioration in quality of life and negatively affects their psycho-emotional state.
- Ulcerative lesions: painful ulcers with a granulation base appear on the skin or mucous membrane.
- Inflammatory process: the ulcers are surrounded by an inflammatory edge, indicating the body’s reaction to infection.
- Bleeding upon trauma: the ulcers may bleed with mechanical impact, worsening the patient’s condition.
- Local pain and itching: the presence of ulcerative lesions is accompanied by anxiety and discomfort in the patient.
- Deterioration of quality of life: the symptoms of the granuloma negatively affect the patient’s psycho-emotional state.
Expert opinion on the treatment of Granuloma inguinale
Experts agree that accurately diagnosing Venereal granuloma is crucial for effective treatment, which includes antibiotic therapy. Determining the sensitivity to antimicrobial agents is a key factor in selecting the optimal treatment regimen, allowing for the avoidance of resistance development and ensuring the effective eradication of the disease pathogen.
Experts advise patients with Venereal granuloma to follow their doctor’s recommendations, adhere to the prescribed course of antibiotics, regularly undergo follow-up examinations, and avoid sexual contact during treatment. Timely consultation with a specialist and strict adherence to prescriptions increase the likelihood of recovery while reducing the risks of complications and the spread of the infection.

Diagnosis of Venereal Granuloma
Diagnosis of Granuloma inguinale includes a clinical examination to identify characteristic signs of this disease, such as the presence of ulcerative lesions with a granulomatous base and inflammatory surrounding. Additionally, a laboratory study of the biopsy material from the affected area is conducted to isolate the bacterium Calymmatobacterium granulomatis, which causes this disease, using specific staining techniques.
When making a diagnosis, it is also important to consider the results of additional laboratory studies, such as microscopic examination of the sampled material, bacteriological cultures, and DNA diagnostics to confirm the presence of the pathogen. Differential diagnosis is conducted with other ulcerative skin diseases, such as chancroid and syphilis, which allows for determining the most effective treatment for this clinical case.
- Clinical examination revealing characteristic ulcerative formations and inflammatory changes on the skin or mucous membranes.
- Laboratory study of biopsy material aimed at identifying the pathogen Calymmatobacterium granulomatis using specific staining methods.
- Microscopic examination of the isolated material to identify characteristic morphological changes and the causative agent of the disease.
- Bacteriological cultures for growing and identifying the pathogen, which is an important method for confirming the diagnosis.
- DNA diagnostics for more accurate identification of the bacterium Calymmatobacterium granulomatis and excluding other infections with a similar clinical picture.
Treatment of Venereal Granuloma
Patients with Venereal Granuloma are advised to have regular follow-ups with a doctor to monitor the effectiveness of treatment, as well as to prevent complications and recurrences of the disease. An important aspect of successful treatment is strict adherence to the doctor’s prescriptions and completing the course of antibiotics to the end to avoid the development of resistance of the pathogen to the medications.
- Systemic use of antibiotics: treatment of Granuloma inguinale typically includes the administration of antibiotics such as doxycycline, erythromycin, or chloramphenicol to eliminate the causative agent.
- Local treatment of the affected area: involves the treatment of ulcerative defects with bactericidal solutions, the use of anti-inflammatory ointments or creams to accelerate healing and reduce the inflammatory process.
- Regular monitoring by a doctor: is recommended for patients with Granuloma inguinale to control the effectiveness of treatment, prevent complications and relapses, and to adjust therapy.
- Strict adherence to doctor’s prescriptions: it is important to complete the course of antibiotics to prevent the emergence of resistance in the causative agent and ensure complete and effective recovery.
- Conducting treatment under the supervision of a specialist: a specialist will help select the optimal treatment, monitor the dynamics of the disease, and respond to any changes in the patient’s condition.
Prevention of Venereal Granuloma
To reduce the spread of Granuloma Inguinale, it is also necessary to detect and treat infected individuals, conduct informational campaigns to prevent sexually transmitted diseases, and raise awareness among both doctors and the public about the symptoms, diagnostic methods, and treatment of this disease.
- Use of condoms: Correct and consistent use of condoms during sexual contacts can significantly reduce the risk of contracting Venereal granuloma.
- Regular screenings: Regular screening for sexually transmitted infections, including Venereal granuloma, allows for early detection of the disease and timely treatment.
- Public education: Conducting information campaigns, educating about safe sex practices, and raising awareness about sexually transmitted diseases contribute to the prevention and control of Venereal granuloma.
- Personal hygiene: Maintaining good hygiene of intimate areas helps prevent the development of infections and reduce the risk of contracting various sexually transmitted diseases, including Venereal granuloma.
- Health monitoring: Regular health monitoring and consulting a doctor upon the appearance of symptoms help to timely identify and treat Venereal granuloma, as well as prevent the spread of the disease.
Interesting aspects of Venereal granuloma
One interesting aspect of Venereal granuloma is its characterization as a “disease of old locations,” as the infection typically occurs in countries with hot and humid climates, where endemic foci are maintained, and in some cases, there may periodically be high morbidity in certain regions.