Decoding human papillomavirus (HPV): features, consequences, and treatment methods
- Understanding the human papillomavirus: key information
- Etiology of human papillomavirus
- The clinical picture of the human papillomavirus.
- Medical assessment of treatment methods for human papillomavirus.
- Methods for diagnosing the human papillomavirus.
- Effective methods for treating human papillomavirus (HPV)
- Measures to prevent human papillomavirus
- Facts and myths about the human papillomavirus
- FAQ
Understanding the human papillomavirus: key information
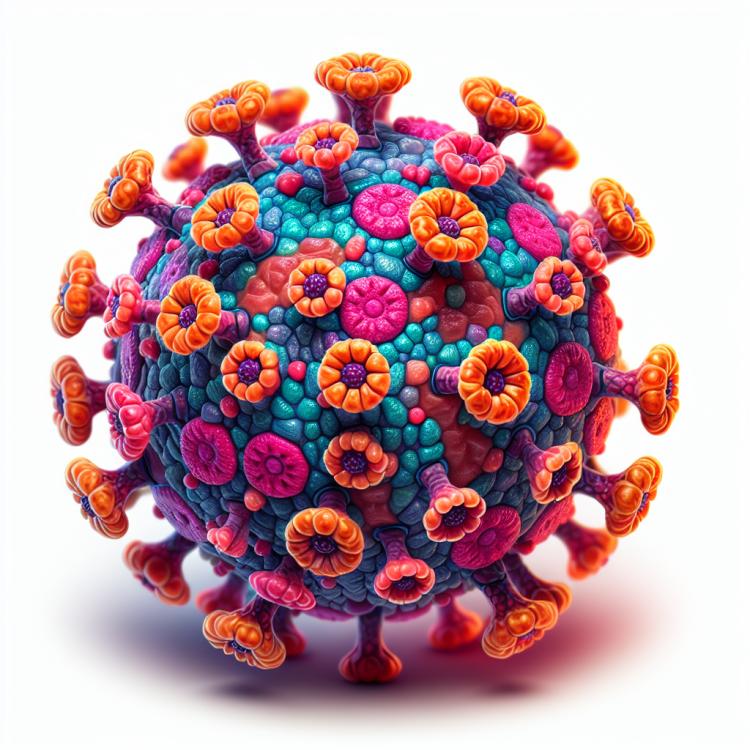
Human papillomavirus (HPV) is a group of viruses that are often transmitted through sexual contact. It can cause undesirable changes in the cells of the skin and mucous membranes, leading to the development of warts, papillomas, and even cervical cancer in women. Understanding the characteristics of HPV, transmission mechanisms, and prevention methods plays a crucial role in preventing diseases associated with this virus and in reducing the risk of its transmission.
Etiology of human papillomavirus
Human papillomavirus (HPV) is a DNA-containing virus that is primarily transmitted through sexual contact. It penetrates through microtraumas into the epithelial cells of the skin and mucous membranes, where it replicates and transforms the cells. Despite the main transmission mechanism being sexual contact, infection can also occur through contact with infected skin or mucous membranes.
The main risk factors for HPV infection are unprotected sexual contact, multiple sexual partners, and low immunity. Certain strains of HPV, such as high-risk strains 16 and 18, have the ability to cause the development of cervical cancer as well as other cancerous diseases. Understanding the etiology of HPV is an important step in preventing the spread of the virus and its serious consequences.
- Human papillomavirus is a DNA-containing virus that is primarily transmitted through sexual contact.
- The transmission of the virus occurs through micro-injuries in the skin and mucous membranes.
- The main risk factors for HPV infection include unprotected sex, multiple sexual partners, and a low immune level.
- High-risk HPV strains, such as 16 and 18, can cause cervical cancer and other oncological diseases.
- Understanding the etiology of HPV is important for medical experts in developing measures to prevent the spread of the virus.
The clinical picture of the human papillomavirus.
The clinical picture of human papillomavirus (HPV) can manifest a variety of symptoms depending on the type of virus, the site of infection, and the overall state of the patient’s immune system. Among the main symptoms, the appearance of warts or papillomas on the skin or mucous membranes, including on the genitals, the anal-genital area, as well as on the mucous membranes of the mouth and throat, should be highlighted. Some high-risk HPV strains can lead to the development of cancerous tumors, especially cervical cancer.
Patients with HPV may also experience various discomforting symptoms such as itching, burning, bleeding, or pain in the affected areas. In addition to visible signs, some carriers of the virus may remain asymptomatic but can still be sources of infection for others. Understanding the clinical picture of HPV allows for timely diagnosis and treatment of the infection, as well as taking measures to prevent and control its spread.
- Appearance of warts and papillomas: one of the typical symptoms of HPV is the formation of warts or papillomas on the skin and mucous membranes.
- Itching and discomfort: patients with HPV may experience itching, burning, or pain in the affected areas, which may be accompanied by bleeding.
- Growth of papillomas in the anogenital area: HPV infection in the anogenital area can lead to the formation of condylomas (vaginal, anal, or penile).
- Occurrence of cancerous tumors: some high-risk strains of HPV are associated with the development of cervical, anal, throat, and other cancers.
- Asymptomatic course: in some carriers of the human papillomavirus, the infection may be asymptomatic, complicating diagnosis and potentially contributing to the spread of the infection.
Medical assessment of treatment methods for human papillomavirus.
Experts in the field of medicine evaluate treatment methods for human papillomavirus (HPV) based on their effectiveness, safety, and accessibility for patients. One of the main treatments for HPV is the use of immunostimulatory drugs, which help strengthen the immune system and fight the virus. This approach allows the body to independently resist the infection and can be particularly effective in cases of low viral activity.
However, alongside immunotherapy, experts also assess the effectiveness of other treatment methods, such as surgical removal of tumors or warts, the use of antiviral drugs, and laser therapy. A thorough medical evaluation of each case of HPV infection allows for the selection of an optimal comprehensive treatment approach, taking into account the individual characteristics of the patient and the characteristics of the virus.

Methods for diagnosing the human papillomavirus.
Diagnosis of human papillomavirus (HPV) includes various methods to detect the presence of the virus or its consequences. One of the main diagnostic methods is molecular genetic analysis, which allows for the identification of specific HPV strains and the detection of high-risk oncogenic strains capable of leading to the development of cancerous tumors. Additionally, investigations for cellular changes caused by the virus can be performed using cytological analysis (Schiller cytology, Papanicolaou cytology) or molecular cytogenetic methods.
Additional diagnostic methods may include colonoscopy, biopsy material analysis, histological examination, as well as recto-sigmoidoscopy. The comprehensive conduct of various diagnostic procedures allows for accurate determination of the presence and nature of human papillomavirus, which in turn assists in selecting the most effective treatment and monitoring of the patient.
- Molecular genetic analysis: identifies specific strains of the human papillomavirus and detects high-risk oncogenic strains capable of causing cancerous tumors.
- Cytological analysis: includes Schiller’s cytology and Papanicolaou cytology to detect cellular changes caused by HPV.
- Molecular cytogenetic methods: help to investigate cellular changes caused by the human papillomavirus.
- Colonoscopy: allows examination of the rectum and detection of possible changes caused by HPV.
- Histological examination: includes analysis of biopsy material for detailed study of tissues and identification of pathologies caused by the virus.
Effective methods for treating human papillomavirus (HPV)
In the case of high-risk oncogenic strains of HPV being detected, treatment may include vaccination to prevent the development of cancer, as well as regular monitoring and diagnosis of tumor processes. The development of new treatment methods and vaccination plays an important role in the fight against HPV and its consequences, as timely intervention significantly reduces the risk of developing cancer-related diseases associated with this virus.
- Cryodestruction: a method based on the use of low temperatures (usually liquid nitrogen) to destroy warts or papillomas caused by HPV.
- Laser therapy: the use of laser radiation to remove affected tissues, which are warts or papillomas on the skin or mucous membranes.
- Surgical removal: a method in which a surgeon removes warts or papillomas using various tools and techniques depending on the location and size of the formations.
- Chemical agents: the use of chemical preparations to act on affected tissues with the aim of removing warts or papillomas caused by HPV.
- Vaccination: the use of vaccines to prevent high-risk oncogenic strains of HPV that can lead to cancer, aimed at reducing the risk of developing oncological diseases.
Measures to prevent human papillomavirus
In addition to vaccination, preventive methods include awareness campaigns about the risks associated with HPV, promoting safe sex, using condoms during sexual contact, regular screening examinations, and early diagnosis of the infection. Adhering to recommendations for HPV prevention and implementing appropriate measures can reduce the likelihood of contracting the virus and lower the risk of developing its complications.
- Vaccination: The vaccine against the human papillomavirus (HPV) is an effective method for preventing infection and the development of cancer related to this virus.
- Information campaign: Conducting informational events about the HPV virus, its consequences, and ways to protect oneself contributes to raising awareness and reducing the risk of infection.
- Safe sex: Practicing safe sex, including the use of condoms, reduces the likelihood of HPV transmission through sexual contact.
- Screening and diagnosis: Regular examinations and diagnostics allow for the detection of the infection in its early stages, which facilitates timely treatment and prevents complications.
- Limiting the number of sexual partners: Reducing the number of partners and establishing long-term relationships also lowers the risk of contracting HPV and other sexually transmitted infections.
Facts and myths about the human papillomavirus
One common myth about HPV is the claim that vaccination against the virus can lead to serious side effects. However, numerous studies confirm the safety and effectiveness of the HPV vaccine in preventing cervical cancer and other virus-related diseases. It is important to clarify the facts about this virus, warn against myths and misinformation, and promote awareness among the population about prevention and treatment measures for HPV.