Viral hepatitis: types, distribution, and prevention
- Basics of Viral Hepatitis
- Common causes of Viral Hepatitis
- Characteristic symptoms of Viral Hepatitis
- Experts’ opinions on the treatment of Viral Hepatitis
- Methods of diagnosing Viral Hepatitis
- Modern approaches to the treatment of Viral Hepatitis
- Prevention measures for Viral Hepatitis
- Interesting facts about Viral Hepatitis
- FAQ
Basics of Viral Hepatitis
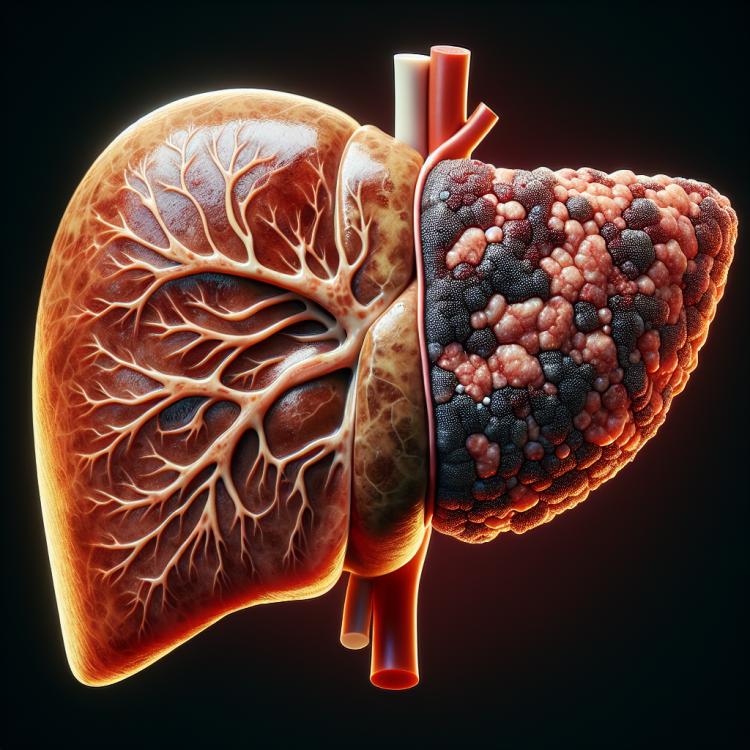
Viral hepatitis is an inflammatory disease of the liver caused by various viruses – hepatitis A, B, C, D, and E. It can manifest in both acute and chronic forms and poses a serious threat to human health. Symptoms of viral hepatitis may include fatigue, discomfort in the liver area, nausea, jaundice, loss of appetite, and other manifestations, which require a comprehensive diagnosis and treatment.
Common causes of Viral Hepatitis
Viral hepatitis occurs as a result of infection with hepatitis viruses A, B, C, D, and E. Viral hepatitis A and E are usually spread through contaminated water or food, while viral hepatitis B, C, and D are transmitted through infected blood or other fluids during contact with contaminated material. One common way to contract viral hepatitis B is through sexual contact with an infected partner, while viral hepatitis C is often transmitted through the use of contaminated needles when using injectable drugs.
- Hepatitis virus infection: Hepatitis viruses A, B, C, D, and E can cause various forms of viral hepatitis.
- Contact with infected blood: Transmission of hepatitis viruses B, C, and D can occur through infected blood via shared needles, blood transfusions, or sexual contact.
- Increased risk of infection: People who abuse drugs or engage in unprotected sex are at an increased risk of contracting viral hepatitis.
- Poor hygiene: Consumption of contaminated water or food can be a source of infection with hepatitis A and E.
- Medical procedures: Failure to adhere to aseptic and antiseptic protocols in medical facilities can lead to the transmission of hepatitis viruses B and C from patient to patient.
Characteristic symptoms of Viral Hepatitis
Characteristic symptoms of viral hepatitis may include fatigue, abdominal pain, loss of appetite, nausea, vomiting, general weakness, weight loss, jaundice (yellowing of the skin and eyes), dark urine, and light-colored stool. Some patients may also experience skin itching, enlargement of the liver and spleen, as well as other symptoms related to impaired liver function.
Viral hepatitis can manifest differently in different people and depending on the type of virus. Some individuals may have only mild symptoms or be asymptomatic, while others may experience more pronounced symptoms that require medical intervention. Early detection and treatment of viral hepatitis is crucial to prevent complications and maintain patient health.
- Fatigue: general weakness and rapid fatigue can be some of the first signs of viral hepatitis.
- Abdominal pain: pain or discomfort in the abdominal area may be associated with liver dysfunction characteristic of hepatitis.
- Loss of appetite: loss of appetite and inability to eat in usual quantities may be a sign of hepatitis.
- Nausea and vomiting: dyspepsia symptoms, including nausea and vomiting, may accompany viral hepatitis.
- Jaundice: the bile pigment bilirubin, accumulated in the body due to impaired liver function, leads to yellowing of the skin and sclera.
Experts’ opinions on the treatment of Viral Hepatitis
Experts in the field of infectious diseases and gastroenterology believe in the importance of early diagnosis and comprehensive treatment of viral hepatitis. Effective treatment approaches for this disease include the use of antiviral medications, supportive therapy to improve liver function, lifestyle change recommendations, and prevention of complications.
Experts also emphasize the importance of the patient’s lifestyle, including healthy eating, moderate physical activity, and the avoidance of harmful habits such as alcohol consumption and smoking, to ensure a successful treatment outcome and overall recovery in cases of viral hepatitis. The treatment strategy is determined individually for each patient, taking into account the type of virus, the extent of liver damage, and other factors, which highlights the significance of a personalized approach in managing this disease.

Methods of diagnosing Viral Hepatitis
Various methods are used for diagnosing viral hepatitis, including blood tests for the presence of viral markers, studying the levels of liver enzymes such as ALT and AST, investigating the viral load, as well as conducting educational procedures such as ultrasound diagnosis of the liver. Additional diagnostic methods may include liver biopsy for a more detailed examination of the extent of liver damage and identifying possible complications.
Accurate and timely diagnosis of viral hepatitis is crucial for determining the type of virus, the degree of liver damage, selecting optimal treatment, and predicting the outcome of the disease. The results of the diagnosis help medical professionals develop an individualized treatment plan for each patient, taking into account the specifics of their condition.
- Blood tests for viral markers: include testing for the presence of antibodies to hepatitis viruses and other viral particles.
- Studying liver enzyme levels: measuring the levels of alanine aminotransferase (ALT) and aspartate aminotransferase (AST) to assess liver function.
- Investigation of viral load levels: determining the number of viral particles in the blood to assess the activity of the infection.
- Educational ultrasound diagnosis of the liver: performing an ultrasound study to determine the size, structure, and condition of the liver.
- Liver biopsy: a procedure for taking a tissue sample from the liver for detailed analysis of the degree of damage and possible complications.
Modern approaches to the treatment of Viral Hepatitis
In addition, direct-acting antiviral (DAA) medications are widely used for viral hepatitis C, targeting the destruction of the virus, which can lead to the cure of the infection. The implementation of a comprehensive treatment approach, including antiviral medications, maintenance of liver function, and monitoring of the overall patient condition, plays an important role in the successful treatment of viral hepatitis.
- Use of antiviral drugs: Modern treatment regimens include the use of antiviral drugs aimed at destroying the hepatitis virus and suppressing its replication.
- Therapy with specific drugs: Specialized drugs are developed for each type of viral hepatitis, aimed at targeting the virus and improving treatment outcomes.
- Use of direct-acting agents: Direct-acting drugs are considered effective for hepatitis C, as they contribute to deep viral suppression and increase the chances of recovery.
- Comprehensive approach to treatment: Specialists often combine various treatment methods, including antiviral drugs, nutritional support, drugs to improve liver function, and monitoring examinations to achieve the best results.
- Individualized approach: Treatment of viral hepatitis is tailored to the patient’s characteristics, the type of virus, the degree of liver damage, and other factors, allowing for optimal results and improved disease prognosis.
Prevention measures for Viral Hepatitis
Preventive measures such as avoiding contact with infected blood and other fluids, using condoms during sexual intercourse, and taking precautions during medical procedures help reduce the risk of hepatitis virus infections. Public education and awareness about the risks and methods of preventing viral hepatitis play a key role in the prevention of diseases in this group.
- Vaccination: Vaccination against hepatitis B is an effective way to prevent infection with this virus.
- Hygiene standards: Adhering to hygiene standards in medical institutions and everyday life helps to prevent infection with hepatitis C viruses.
- Food and water safety: Following hygiene norms when preparing food and consuming drinking water helps to avoid infection with hepatitis A and E through contaminated sources.
- Avoiding contact with infected blood: Avoiding contact with infected blood and other contaminated fluids reduces the risk of hepatitis virus infection.
- Organization of educational events: Conducting educational campaigns about the risks of infection and methods of preventing viral hepatitis contributes to raising public awareness and taking necessary preventive measures.
Interesting facts about Viral Hepatitis
Moreover, viral hepatitis A and E are typically transmitted through contaminated water and food, especially in conditions of poor hygiene, which reflects the importance of following preventive measures to avoid infection with these types of viral hepatitis.