Prolapse of the rectum: symptoms, causes, and treatment
- Definition and Causes of Rectal Prolapse
- Pathophysiology and risk factors in rectal prolapse
- Clinical picture of rectal prolapse
- Expert recommendations for the treatment of rectal prolapse
- The role of diagnosis in determining rectal prolapse
- Methods of treating rectal prolapse
- Tips for preventing rectal prolapse
- Amazing aspects of rectal prolapse
- FAQ
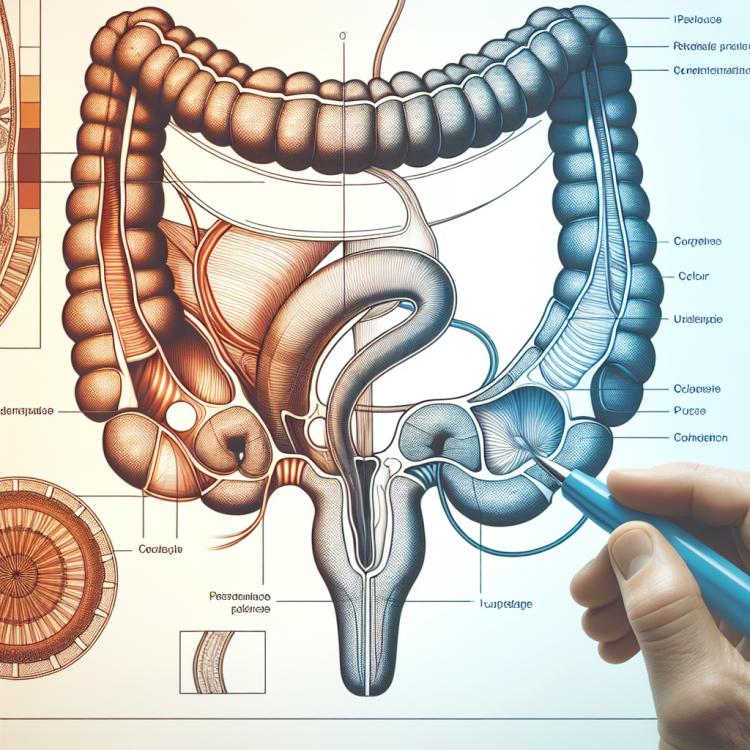
Definition and Causes of Rectal Prolapse
Rectal prolapse, also known as rectal prolapse, is a condition in which part of the rectum protrudes and bulges through the anal opening. One of the main causes of rectal prolapse is the weakening of the ligaments and muscles that support the rectum in position. This defect becomes particularly noticeable during pressure on the abdomen during defecation or physical exertion. It should be noted that rectal prolapse usually does not occur on its own but can be the result of various factors, including chronic constipation, childbirth procedures, chronic cough, or trauma.
Pathophysiology and risk factors in rectal prolapse
Rectal prolapse, or rectoptosis, occurs due to the weakening of the ligaments and muscles that support the rectal tissue, leading to its displacement and protrusion through the anus. Causes may include factors such as aging, childbirth, chronic straining during defecation, obesity, and chronic prolapsing. Other risk factors include chronic constipation, trauma, surgical interventions in the pelvic or rectal area, as well as a lack of physical activity.
In addition to this, developmental anomalies, disturbances in intra-abdominal pressure, and abnormalities in muscle tone may also contribute to the causes of rectoptosis. Effective understanding of the pathophysiology and identification of risk factors are important steps in the diagnosis and treatment of this condition, providing a basis for selecting the most appropriate management approach for the patient.
- Weakening of ligaments and muscles: Injury or aging can lead to the weakening of structures that support the rectal tissue, contributing to rectal prolapse.
- Aging: As tissues and muscles become less elastic with age, the risk of rectal prolapse increases.
- Childbirth: Labor can cause stretching and damage to the pelvic floor tissues, increasing the likelihood of developing rectocele.
- Chronic straining during defecation: Constant straining during the act of defecation can lead to weakening of the muscles and ligaments in the rectal area.
- Obesity: Excess weight can increase internal pressure in the abdominal cavity, contributing to rectal prolapse.
Clinical picture of rectal prolapse
When rectal prolapse occurs, patients may experience various symptoms, including a feeling of discomfort or heaviness in the rectal area, especially during prolonged standing or walking. Manifestations may include a sense of external pressure or even the “prolapse” of tissue through the anus. Patients may also report increased pain in the rectal area, exacerbated by physical activity or defecation.
Other common symptoms of rectal prolapse include periodic involuntary bowel movements or worsening fecal control, which can lead to discomfort or psychosocial issues for the patient. Pain and discomfort in the rectal area, as well as changes in bowel patterns, may be grounds for seeking medical advice for further evaluation and management of this issue.
- Discomfort and heaviness in the rectal area: patients may experience discomfort and pressure in the rectal area, especially during long periods of standing or walking.
- Tissue prolapse through the anus: a sensation of tissue or organ protruding through the anus may occur with rectal prolapse.
- Pain in the rectal area: patients may report increased pain in the rectal area, worsening with physical activity or during defecation.
- Fecal incontinence: may manifest as occasional involuntary defecation or worsening control over bowel movements.
- Psychosocial issues: the presence of rectal prolapse symptoms can lead to psychological and social problems for the patient.
Expert recommendations for the treatment of rectal prolapse
Experts in the field of coloproctology emphasize the importance of an individualized approach to the treatment of rectal prolapse, considering various factors such as age, degree of prolapse, presence of comorbidities, and the overall condition of the patient. Treatment may include conservative methods, such as lifestyle change recommendations, exercises to strengthen the pelvic floor muscles, physiotherapy, and regulation of defecation. For some patients, surgical intervention may be required, including rectopexy or other procedures to strengthen tissues and stabilize the rectum.
Expert feedback is positively inclined towards the use of multimodal approaches, which may include a combination of conservative and surgical methods to achieve the best treatment outcomes for patients with rectal prolapse. It is important to emphasize that early diagnosis and timely initiation of treatment are key in preventing complications and improving the prognosis for patients with this condition.

The role of diagnosis in determining rectal prolapse
The diagnosis of rectal prolapse plays an important role in determining this condition and developing a treatment plan for each patient. During the diagnosis, the doctor may perform a physical examination, take a medical history, and conduct a rectal examination to assess the degree of prolapse and the causes of this disorder. Additional methods such as ultrasound, CT, or MRI can help clarify the diagnosis and determine the extent of the pathology.
In addition to examinations, educational moments play an important role in diagnosing rectoptois, as they provide patients with understanding and informed consent for subsequent treatment. Diagnosis helps the doctor and patient develop a personalized treatment plan, taking into account the patient’s condition and the severity of rectal prolapse.
- Physical examination: examination of the rectum allows for assessing the degree of prolapse and establishing a diagnosis.
- Medical history: gathering a complete medical history of the patient helps identify possible causes and risk factors for rectal prolapse.
- Additional methods: conducting ultrasound, CT, or MRI helps clarify the diagnosis and determine the extent of the pathology.
- Educational moments: informing the patient about diagnostic procedures and their importance contributes to understanding and agreeing to treatment.
- Individualized approach: diagnosing rectal prolapse allows for developing a personalized treatment plan considering the characteristics of each patient.
Methods of treating rectal prolapse
An individualized approach to the treatment of rectal prolapse is necessary for each patient, taking into account all aspects of their condition and ensuring optimal outcomes. Effective treatment of this disorder should include a combination of medication therapy, physiotherapy, surgical techniques, and ongoing monitoring of the patient to prevent recurrences and maintain their long-term health.
- Conservative methods: Include physical therapy to strengthen the pelvic floor muscles, dietary changes to ease defecation, and the use of anti-inflammatory medications if necessary.
- Surgical intervention: In cases where conservative methods are ineffective, surgical correction may be needed, such as rectopexy or rectal fixation.
- Biofeedback and physiotherapy: Used to improve muscle tone and control over the pelvic muscles, which can help prevent further rectal prolapse.
- Sclerotherapy injections: This method may be used to harden the tissues around the anus and prevent rectal prolapse.
- Proctological exercises: Developing proper defecation mechanics and strengthening the pelvic floor muscles through special exercises may be an important component of treatment.
Tips for preventing rectal prolapse
In addition, preventing tissue damage to the rectum during heavy lifting and avoiding excessive pressure during defecation will also help reduce the risk of organ prolapse. Patients with risk factors, such as obesity, chronic constipation, or childbirth, are advised to undergo regular medical check-ups for timely detection and monitoring of rectal conditions.
- Maintain a healthy lifestyle: lead an active lifestyle, control your weight, and regularly engage in exercises to strengthen the pelvic floor muscles.
- Watch your diet: consume fiber-rich foods and drink enough fluids to maintain normal peristalsis and prevent constipation.
- Avoid excessive straining: try not to push too hard during the act of defecation to avoid creating excessive pressure in the rectal area.
- Reduce the risk of injury: prevent the possibility of tissue damage to the rectum when lifting heavy objects and during other daily activities.
- Schedule regular check-ups: if you have risk factors for rectal prolapse, consult a doctor for medical examinations and monitoring of the organ’s condition.
Amazing aspects of rectal prolapse
In addition to this, it is important to realize that early detection and adequate treatment of rectoplexy can greatly improve the quality of life for the patient and prevent potential complications. Collaborative efforts between healthcare professionals and the patient in conducting interactions and preventing this disorder can lead to a significant reduction in the risk of rectal prolapse and its consequences.