Achondroplasia: symptoms, causes, and modern treatment methods
- Understanding Achondroplasia: Definition, Causes, and Features
- Factors for the occurrence of Achondroplasia
- Clinical picture of Achondroplasia
- Expert opinion on the treatment of achondroplasia
- Methods for diagnosing Achondroplasia
- Methods of treating Achondroplasia
- Measures for the prevention of achondroplasia
- Amazing aspects of achondroplasia
- FAQ
Understanding Achondroplasia: Definition, Causes, and Features
Achondroplasia is a genetic disorder characterized by abnormalities in the growth of bones and cartilage. It is caused by mutations in genes responsible for the synthesis of cartilage tissue. Patients with achondroplasia often have short stature, skeletal deformities, and other medical issues. The exact causes of this genetic disorder are not fully understood, however, research in the field of molecular genetics allows for a deeper understanding of the mechanisms underlying the development of achondroplasia.
Factors for the occurrence of Achondroplasia
Achondroplasia is a genetic disorder caused by mutations in the gene that encodes for the IGF-1 growth factor receptor. This receptor plays a key role in regulating the growth of bones and tissues. Mutations in this gene can reduce the receptor’s activity, leading to impaired bone growth and the typical symptoms of achondroplasia.
In addition to genetic factors, achondroplasia can also be caused by random mutations or new sporadic mutations occurring in a child without regard to inheritance from parents. Understanding these factors is crucial for the diagnosis and development of treatment strategies for achondroplasia.
- Genetic mutations: Mutations in the gene encoding the IGF-1 growth factor receptor are the primary cause of achondroplasia.
- Spontaneous mutations: Sometimes achondroplasia can occur due to random mutations or new changes in genes not related to heredity.
- Heredity: Parental genes can be passed down and become a cause of achondroplasia due to inherited traits.
- Role of the IGF-1 growth factor: Disorders in the functioning or activity of the IGF-1 growth factor receptor can contribute to the development of this genetic disease.
- Gene interactions: The complex interaction between different genes may also play a role in the emergence of achondroplasia, although the exact mechanisms of this process require further research.
Clinical picture of Achondroplasia
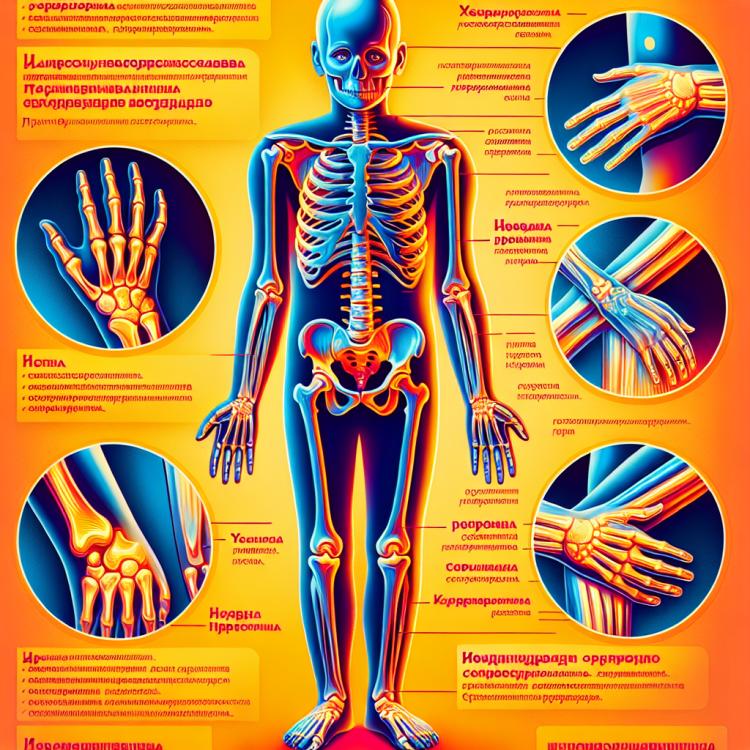
Achondroplasia is a genetic disorder of cartilage and bone, characterized by short stature and a distinctive appearance. Clinical manifestations vary depending on the type of achondroplasia, but typically include short limbs, disproportionate head and trunk sizes, bone deformities, and limited joint mobility.
Additionally, symptoms of achondroplasia may include a concave chest, delays in social skills development in children, and vision and hearing problems. Children with achondroplasia require an individualized approach in medical and rehabilitative care, highlighting the importance of providing comprehensive attention in managing this condition.
- Short extremities: one of the main clinical signs of achondroplasia is the underdevelopment of the extremities, which leads to significant shortening of growth.
- Discrepancy between head and torso size: children with achondroplasia often have a normal head size, while the torso remains short and compact, creating a disproportion in physical development.
- Bone deformities: patients with achondroplasia may experience bone deformities such as bowed legs, twisted limbs, and other skeletal anomalies.
- Limited joint mobility: due to changes in the structure of bones and cartilage, patients with achondroplasia may face limitations in joint mobility.
- Vision and hearing problems: some children with achondroplasia may experience vision problems, such as strabismus, or hearing issues due to skull bone anomalies.
Expert opinion on the treatment of achondroplasia
Experts in pediatrics and genetics emphasize the importance of early detection and a personalized approach to the treatment of achondroplasia. Standard treatment for achondroplasia includes a range of strategies, such as physical therapy to strengthen muscles and improve mobility, as well as surgical interventions to correct bone deformities. However, the effectiveness of therapy may vary depending on the individual characteristics of each patient.
Experts believe that a multidisciplinary approach to the treatment of achondroplasia, involving physicians from various specialties such as orthopedists, endocrinologists, and geneticists, can enhance the effectiveness of therapeutic measures. Gene therapy also represents a promising approach in the treatment of achondroplasia, but it requires further research and clinical trials to determine its effectiveness and safety.

Methods for diagnosing Achondroplasia
Diagnosis of achondroplasia includes studying the clinical manifestations of the disease, radiological examination of the bones to identify characteristic deformities and growth disorders, as well as genetic tests to detect mutations in the gene responsible for the development of the pathology. A comprehensive approach to diagnosis allows for an accurate diagnosis and the establishment of an appropriate treatment plan.
Additionally, the use of medical imaging methods, such as magnetic resonance imaging (MRI) and computed tomography (CT), can be helpful for a detailed examination of changes in tissues and assessing the degree of damage to organs and systems in the body in cases of achondroplasia. The rational application of diagnostic methods plays an important role in determining the treatment strategy and prognosis of the disease.
- Clinical examination: The doctor conducts a physical examination of the patient for characteristic symptoms of achondroplasia, such as short limbs and disproportionate sizes of the torso and head.
- X-ray: Radiological examination is used to visualize skeletal deformations, stagnant changes in the bones, and growth disorders of the bones.
- Genetic testing: Determination of mutations in the IGF-1 receptor gene can be performed to confirm the diagnosis of achondroplasia and identify hereditary factors.
- Magnetic resonance imaging (MRI): A highly sensitive method of investigation that allows detailed visualization of changes in soft tissues and joints, which can be useful in the diagnosis of achondroplasia.
- Computed tomography (CT): Used to obtain more detailed images of bones and tissues, which helps specialists to more accurately determine lesions and the severity of achondroplasia.
Methods of treating Achondroplasia
An expert team specializing in the treatment of achondroplasia typically develops an individualized approach for each patient, taking into account the clinical picture, possible complications, and support needs. Continuous monitoring and support for patients with achondroplasia play a crucial role in improving their quality of life and reducing the severity of the symptoms of this genetic disorder.
- Surgical intervention: In cases of achondroplasia, surgical correction of bone or joint deformities may be required to improve mobility and functionality.
- Physical therapy: Physiotherapy and specialized exercises can help improve muscle tone, coordination, and overall physical condition of patients with achondroplasia.
- Medication: Medications may be used to reduce pain, improve sleep quality, maintain bone health, and address other aspects of medical care.
- Rehabilitation and therapeutic services: A comprehensive rehabilitation program includes not only physical therapy but also social and psychological support for patients and their families.
- Individualized approach: Since achondroplasia manifests with diverse symptoms and complications, treatment often requires an individualized approach tailored by specialists for each specific case.
Measures for the prevention of achondroplasia
-
– Genetic counseling: Regular consultations with a genetic specialist help families with a history of achondroplasia make informed decisions about pregnancy planning and the risk of passing on genetic disorders to offspring.
– Genetic testing: Conducting genetic tests to determine the presence of mutations associated with achondroplasia can help identify the risk of inheriting the disease.
– Educational programs: Organizing educational events for patients with achondroplasia and their families helps improve understanding of the disease, treatment methods, and preventive measures.
– Psychological support: Providing psychological assistance to patients and their families can reduce psychosocial stress related to the diagnosis and treatment of achondroplasia.
– Research and clinical trials: Conducting research in genetics and medicine helps develop new methods for diagnosing, treating, and preventing achondroplasia.
Amazing aspects of achondroplasia
Moreover, achondroplasia is also interesting in the context of socio-psychological aspects. Children suffering from this genetic disorder may experience difficulties in adapting to society due to their appearance and physical limitations. Working with such patients requires a unique approach that addresses not only their medical needs but also their psychological well-being and social integration.