Ascites: possible causes, symptoms, and treatment methods
Understanding ascites: symptoms, causes, and treatment
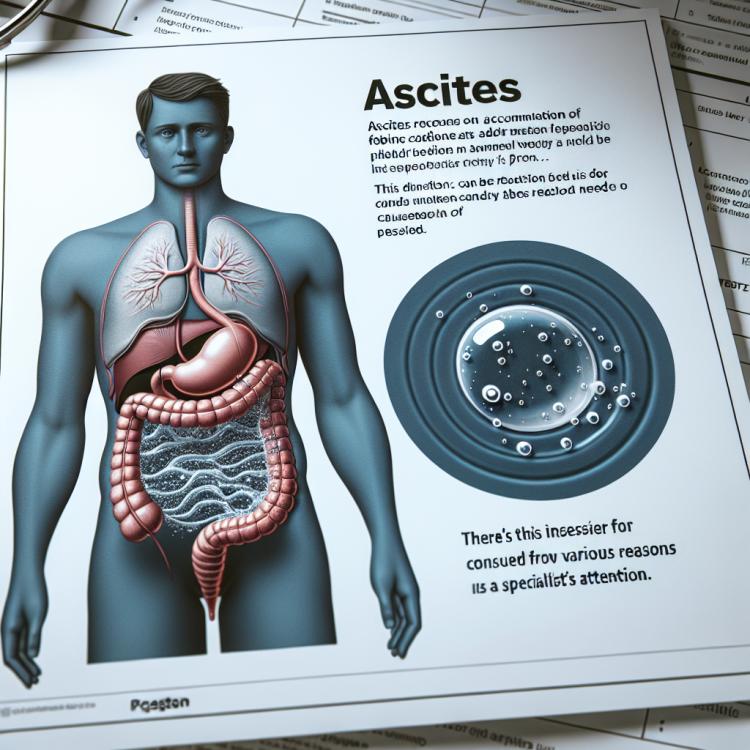
Ascites is a pathological condition characterized by the accumulation of fluid in the abdominal cavity. One of the main symptoms of ascites is an increased abdominal volume caused by fluid accumulation. Based on the mechanism of development, ascites is classified into transudative and exudative variants, which have different causes, including liver cirrhosis, peritoneal cancer, and heart failure. Treatment of ascites depends on its cause and may include a salt-restricted diet, the use of diuretics, and in some cases, surgical intervention.
Etiology of ascites
Ascites, the accumulation of fluid in the abdominal cavity, is a consequence of various pathological conditions such as liver cirrhosis, heart failure, cancer, and inflammatory processes in the abdominal cavity. In patients with liver cirrhosis, ascites is most commonly caused by increased pressure in the venous system of the liver and an imbalance between fluid and sodium ion.
Other common causes of ascites include congestive heart failure, where weak heart function leads to reduced blood flow throughout the body and fluid retention in the tissues. Cancer, especially front abdominal cancer, can also be a cause of ascites due to metastases in the abdominal cavity or compression of lymphatic vessels.
- Liver cirrhosis: cirrhosis often leads to the formation of ascites due to increased pressure in the venous system of the liver and an imbalance in fluid and sodium levels.
- Heart failure: this can lead to ascites due to a decreased ability of the heart to pump blood and fluid retention in the tissues.
- Cancer: tumors in the abdominal cavity or metastases in this area can cause ascites by compressing lymphatic vessels and the abdominal cavity.
- Inflammatory diseases: such as peritonitis or pancreatitis can lead to the formation of ascites due to inflammation in the abdominal cavity.
- Portal hypertension: increased pressure in the venous subsystem through the liver can cause ascites in patients with liver pathology.
Clinical manifestations of ascites
Ascites, characterized by the accumulation of fluid in the abdominal cavity, causes various clinical manifestations. Patients with ascites often experience swelling in the abdominal area, which may become noticeable even in the early stages of the disease. The abdominal area may be tense and round due to fluid accumulation, and this may be accompanied by discomfort or pain.
It is useful to pay attention to observed changes in the size of the patient’s abdomen, especially if they appear suddenly or increase rapidly. Additional symptoms may include loss of appetite, fatigue, shortness of breath, a feeling of heaviness in the abdomen, and unusual sweating. Additionally, ascites can lead to decreased urination, swelling of the legs and ankles, and a general feeling of breathlessness.
- Abdominal swelling: accumulation of fluid in the abdominal cavity can lead to an increase in the volume of the abdomen and swelling in its area.
- Tightness of the abdominal wall: due to fluid accumulation, the abdominal wall may become hard and tense.
- Discomfort and pain sensations: patients often feel discomfort or pain in the abdominal area due to ascites.
- Loss of appetite: ascites may be accompanied by loss of appetite, which can lead to a reduction in food intake.
- Fatigue and shortness of breath: patients with ascites often complain of fatigue, shortness of breath, and a general feeling of weakness.
Comments from specialists on ascites treatment
Experts in the fields of hepatology and oncology emphasize the importance of an individualized approach to the treatment of ascites, taking into account the underlying disease, the patient’s predisposition, and the dynamics of clinical manifestations. For patients with liver cirrhosis, the main treatment goals are to control ascites, improve liver function, and prevent complications such as infections or hemorrhages.
The use of diuretics, a low-salt diet, paracentesis (removal of fluid from the abdominal cavity), and in some cases transjugular intrahepatic portosystemic shunt (TIPS) may be proposed treatment options. Experts also highlight the importance of regular monitoring of the patient’s condition, adjusting therapy based on the dynamics of the disease, and taking measures to prevent recurrences of ascites.

Methods of diagnosing ascites
The diagnosis of ascites is a complex process that typically includes a physical examination of the patient, as well as various instrumental and laboratory studies. During the physical examination, the doctor pays attention to signs of fluid in the abdominal cavity, such as a distended abdomen or the “shifting dullness” sign when tapping. Signs of underlying conditions that may contribute to the development of ascites, such as liver failure or heart failure, are also assessed.
Instrumental diagnostic methods for ascites may include ultrasound of the abdominal cavity, computed tomography (CT), or magnetic resonance imaging (MRI) to visualize the fluid and evaluate the abdominal organs. Laboratory tests, such as analysis of the abdominal fluid (paracentesis), can help identify the cause of ascites, determine the composition of the fluid, and rule out infection. A comprehensive approach to diagnosis ensures an accurate assessment of the patient’s condition and allows doctors to choose the most effective treatment.
- Physical examination: the doctor conducts an examination and palpation to determine the presence of signs of fluid in the abdominal cavity, such as abdominal distension and changes in sound during percussion.
- Ultrasound examination: performed to visualize fluid in the abdominal cavity, determine its volume, and assess the condition of the internal organs.
- Computed tomography (CT): an imaging method that allows for a more detailed study of the structures within the abdominal cavity, determining the cause of ascites.
- Magnetic resonance imaging (MRI): allows for more accurate images of the internal organs and fluid in the abdominal cavity.
- Analysis of abdominal cavity fluid (puncture): conducted to assess the composition of the fluid, identify possible infections, and determine the underlying disease.
Methods of treating ascites
More invasive treatment methods, such as transjugular intrahepatic portosystemic shunt (TIPS), as well as surgical interventions to reduce pressure in the abdominal cavity, may also be employed. Effective treatment of ascites requires an integrated approach and consideration of the specifics of each individual case to achieve the best outcomes and prevent possible complications.
- Diet with salt restriction: low-salt eating helps reduce fluid retention in the body and lower pressure in the abdominal cavity.
- Diuretics: medications in this class help encourage the kidneys to eliminate excess fluid, which contributes to reducing ascites.
- Paracentesis: puncturing the abdominal cavity allows for the removal of accumulated fluid, easing breathing and reducing abdominal volume.
- Treatment of the underlying condition: successful management of ascites often requires treating the underlying condition, such as liver cirrhosis, cancer, or heart failure.
- TIPS procedure: transjugular intrahepatic portosystemic shunt can be applied in certain cases to reduce pressure in the abdominal cavity.
Measures for the prevention of ascites
The main focus should be on adhering to the doctor’s recommendations regarding the treatment of the underlying condition and taking prescribed medications. If the first signs of ascites are detected, it is important to consult a doctor for timely diagnosis and treatment, which will help prevent disease progression and reduce the risk of severe complications.
- Following a low-salt diet: to reduce fluid retention in the body and prevent ascites, it is important to follow a low-salt diet as recommended by a doctor.
- Regular medical supervision: patients with underlying conditions that contribute to the development of ascites should undergo regular medical check-ups for timely detection and monitoring of their condition.
- Monitoring abdominal pressure: maintaining stable abdominal pressure can help prevent fluid accumulation and the development of ascites.
- Adhering to doctor’s recommendations: it is important to follow the physician’s instructions regarding the treatment of the underlying condition and the intake of prescribed medications to prevent the occurrence of ascites.
- Timely consultation with a doctor at the first signs: upon noticing signs of ascites, it is important to seek medical help immediately for diagnosis and treatment, which will help prevent complications and improve the disease prognosis.
Funny facts about asceticism
Another interesting fact about ascites is that this symptom can exist as a standalone condition or be associated with other diseases. For example, ascites can be one of the signs of liver cirrhosis or heart failure, but it can also arise due to abdominal cancer or infections. Studying these aspects helps improve the understanding of ascites and develop more effective treatment methods.