Intestinal candidiasis: causes, symptoms, and effective treatment
- Definition and symptoms of intestinal candidiasis
- Etiology of intestinal candidiasis
- The clinical picture of intestinal candidiasis
- Medical opinion on the treatment of intestinal candidiasis
- Methods of diagnosing intestinal candidiasis
- Principles of treating intestinal candidiasis
- Prevention measures for intestinal candidiasis
- Information about Candida and intestinal candidiasis
- FAQ
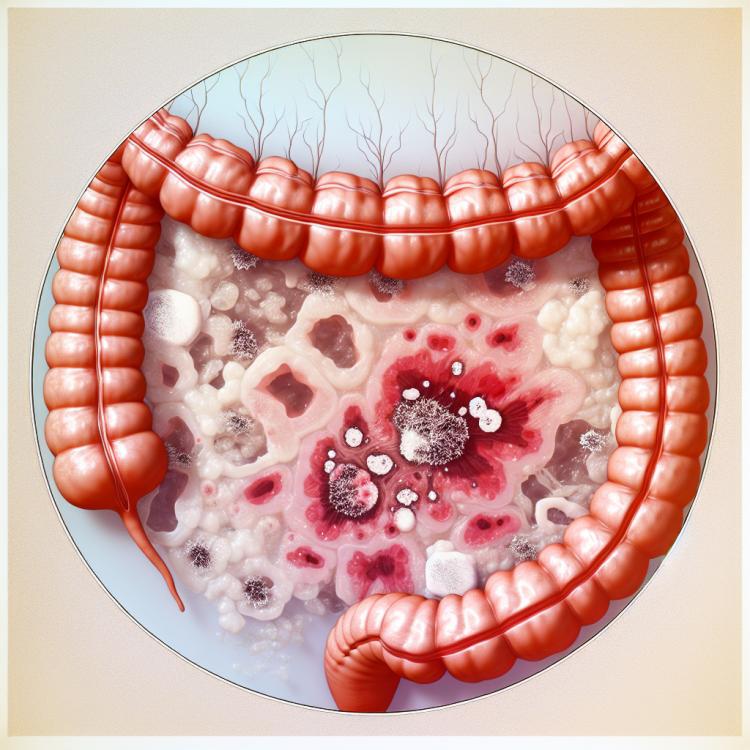
Definition and symptoms of intestinal candidiasis
Intestinal candidiasis is a fungal infectious disease caused by the yeast-like fungus Candida spp. This pathological process can lead to various clinical manifestations, including diarrhea, bloating, abdominal pain, and digestive disorders. The symptoms of intestinal candidiasis can often be masked by other diseases, complicating diagnostics and requiring a comprehensive approach to patient examination.
To establish an accurate diagnosis of intestinal candidiasis, microbiological studies are necessary, including stool tests for the presence of fungi and DNA testing to identify species of Candida spp. Accurate identification of symptoms and timely treatment can help prevent the development of complications and ensure successful recovery of the patient.
Etiology of intestinal candidiasis
Intestinal candidiasis is caused by the yeast-like fungus Candida, the main species of which are Candida albicans, Candida glabrata, and Candida tropicalis. Conditions that promote the development of intestinal candidiasis include prolonged use of antibiotics, immunodeficient states (such as HIV infection), diabetes, as well as malnutrition, pregnancy, and stressful situations. These factors create a favorable environment for the increase of Candida populations in the intestine and the development of the disease.
- Antibiotic use: prolonged use of antibiotics can disrupt the natural gut microbiome and promote the growth of Candida.
- Immunodeficiency states: reduced immunity, such as in HIV infection or other immunodeficiency states, increases the risk of developing intestinal candidiasis.
- Diabetes: patients with diabetes have an increased risk of candidiasis due to metabolic disorders and immune deficiency typical of this condition.
- Malnutrition: deficiencies in nutrients and trace elements can weaken the body’s protective functions, making it more vulnerable to infections, including candidiasis.
- Pregnancy: changes in a woman’s hormonal background and immune system during pregnancy can contribute to the development of intestinal candidiasis.
The clinical picture of intestinal candidiasis
The clinical picture of intestinal candidiasis may include symptoms such as diarrhea, bloating, abdominal pain, and nonspecific digestive disorders. Patients may also experience weakness, loss of appetite, weight, decreased energy, and stool abnormalities. Depending on the extent of intestinal damage by the Candida fungus, clinical manifestations can vary from mild nonspecific complaints to more serious symptoms requiring comprehensive treatment.
- Diarrhea: one of the main symptoms of intestinal candidiasis is the possible presence of sharp and frequent diarrhea, which may be accompanied by watery stools.
- Bloating: due to digestive disturbances and intestinal activity, patients with intestinal candidiasis may experience a feeling of bloating and discomfort.
- Abdominal pain: some people with the disease may experience different types of abdominal pain, including cramps and malaise.
- Nonspecific digestive disorders: symptoms may include nausea, vomiting, unsatisfactory digestion, and a bad taste in the mouth.
- General symptoms: weakness, loss of appetite, weight, decreased energy, and bowel disturbances may be characteristic of intestinal candidiasis.
Medical opinion on the treatment of intestinal candidiasis
The medical community is of the opinion that for the successful treatment of intestinal candidiasis, a comprehensive approach is necessary, including antifungal therapy, normalization of intestinal microbiota, as well as adherence to a diet and eating regimen. The main method of treatment is the use of antimycotic drugs, such as fluconazole, itraconazole, or fluconazole. Experts also recommend using probiotics to restore the balance of microorganisms in the intestines and improve the immune defense of the body.

Methods of diagnosing intestinal candidiasis
To diagnose intestinal candidiasis, various methods are used, including microscopy of preparations, culture studies on nutrient media to grow Candida spp., as well as molecular genetic tests to identify the genetic materials of fungi in samples. In addition, doctors may perform a biopsy of the intestine followed by examination of tissue samples under a microscope to confirm the diagnosis of intestinal candidiasis. The combination of different diagnostic methods allows for the accurate determination of the presence of a fungal infection in the intestine and the appointment of appropriate treatment.
- Microscopy of samples: The method includes studying biot material samples under a microscope to detect fungal structures.
- Cultural studies: Growing Candida spp. on nutrient media for identification and determining sensitivity to antifungal therapy.
- Molecular genetic tests: Analyzing the genetic material of fungi for accurate identification of Candida spp. in samples.
- Intestinal biopsy: Examination of tissue samples from the intestine taken during biopsy to confirm the presence of fungal infection.
- Immunological tests: Using antibody analysis or other markers in the blood for the diagnosis of intestinal candidiasis.
Principles of treating intestinal candidiasis
In some cases, prebiotics and probiotics may be prescribed to restore healthy intestinal microflora. A comprehensive approach that includes medication, dietary corrections, and normalization of microflora helps effectively deal with intestinal candidiasis.
- Application of antifungal drugs such as fluconazole or itraconazole to suppress the growth of Candida in the intestine.
- Correction of factors that create favorable conditions for the development of candidiasis, such as eliminating dysbiosis and boosting immunity.
- Adherence to a diet that excludes foods that contribute to the increase of fungal flora in the intestine.
- Prescription of prebiotics and probiotics to restore healthy microflora and maintain balance in the intestine.
- A comprehensive approach to treatment, including medication therapy, diet, and normalization of microflora, helps effectively combat intestinal candidiasis.
Prevention measures for intestinal candidiasis
To prevent intestinal candidiasis, it is recommended to practice hand hygiene, avoid using shared towels and dishes with infected individuals, especially when immunodeficiencies are present. Strengthening immunity through a healthy lifestyle, regular physical exercise, adequate rest, and moderate alcohol consumption helps reduce the risk of developing intestinal candidiasis.
- Maintaining a healthy gut microflora: The diet should be diverse, including foods rich in prebiotics and probiotics to promote the growth of beneficial bacteria.
- Prudent use of antibiotics: Avoid excessive and non-targeted use of antibiotics, as this can disrupt the balance of intestinal microflora, creating conditions for the development of intestinal candidiasis.
- Maintaining hygiene: Regular hand washing, avoiding shared dishes and towels with infected individuals helps prevent the transmission of fungal infections.
- Strengthening immunity: A healthy lifestyle, including regular physical exercise, sufficient sleep, a balanced diet, and limiting alcohol consumption, contributes to strengthening the immune system and reducing the risk of intestinal candidiasis.
- Prevention in immunocompromised conditions: Patients with immune system disorders should take special care in preventing intestinal candidiasis, taking necessary measures under medical supervision to reduce the risk of infection.