Meibomianitis: signs, diagnosis, and effective treatment
- Definition and essence of meibomian gland
- Factors contributing to the development of meibomitis
- Clinical picture of meibomitis
- The specialists’ view on meibomitis therapy
- Methods for detecting meibomitis
- Principles of meibomian gland dysfunction therapy
- Measures to prevent meibomitis
- Amazing aspects of meibomian glands
- FAQ
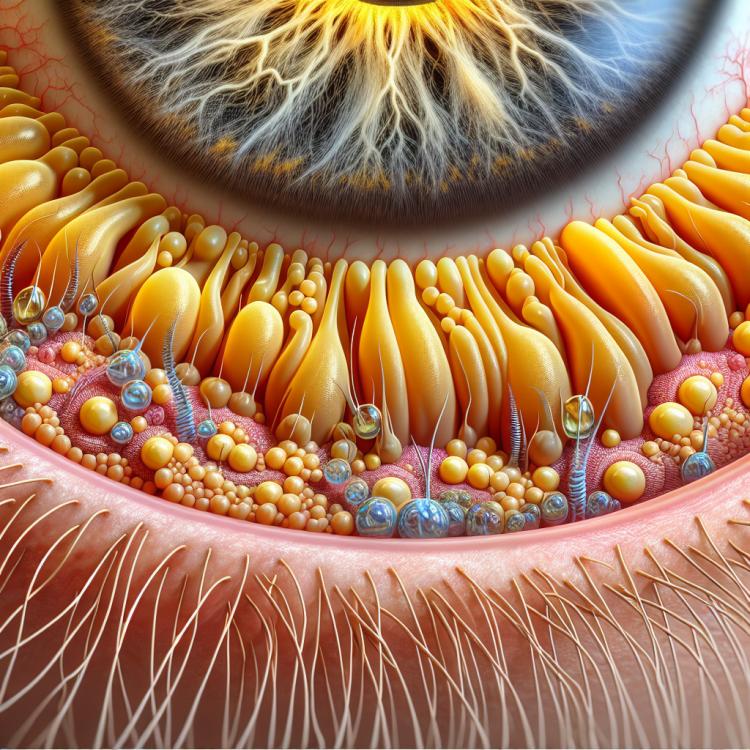
Definition and essence of meibomian gland
Meibomitis is an inflammatory disease of the ducts of the meibomian glands, responsible for producing the oil needed to moisturize the surface of the eyeball. As a result of the inflammation, the gland becomes blocked and infected, leading to symptoms of eye irritation, covering films, and pain. The diagnosis of meibomitis is based on clinical manifestations, including examination of the eyelids and surrounding tissues, as well as the medical history.
The disease usually responds to conservative treatment, which includes warm compresses, massage, and the use of antibiotics or anti-inflammatory drops. In cases of chronic meibomitis or recurrences, surgical intervention may be required, such as gland removal. To prevent the recurrence of the disease, it is important to follow hygiene rules, regularly clean the eyelids, and adhere to the doctor’s recommendations for eye care.
Factors contributing to the development of meibomitis
Meibomitis, a chronic inflammation of the meibomian glands of the eyelids, can develop due to impaired secretion of these glands. One of the reasons for this is the difficult outflow of sebaceous secretions from the meibomian glands due to their diseases or anatomical features. Increased viscosity of the secretion, thinning of the mucous membrane of the gland duct, or stagnation of the secretion due to diseases of the eyelids and adjacent tissues are also possible.
- Disruption of gland secretion: diseases of the meibomian glands or anatomical changes can lead to difficulty in the outflow of sebum.
- Increased viscosity of secretion: increased viscosity of the sebaceous secretion can contribute to stagnation and the development of inflammation in the meibomian glands.
- Thinning of the mucous membrane of the gland duct: in this condition, damage to the walls of the gland and the formation of blockages may occur.
- Stagnation of secretion: in diseases of the eyelids and periorbital tissues, stagnation of secretion may be observed, which promotes the proliferation of bacteria.
- Increased sensitivity of the skin around the eyes: especially in individuals with heightened skin sensitivity around the eyes, the risk of developing meibomitis may be higher.
Clinical picture of meibomitis
The clinical picture of meibomitis is usually characterized by localized inflammation in the edge tissues of the eyelids, near the meibomian glands. Patients may complain of pain, swelling, and hyperemia of the conjunctiva, sometimes with a foreign body sensation. Additionally, purulent discharge from the meibomian duct may occur, as well as the formation of a characteristic coating on the eyelid.
The symptoms of meibomitis may also include spasmodic contractions of the eyelid muscles, itching, a burning sensation, and redness of the eyelid skin. Sensitization of the eyelids to light and a general decrease in well-being are often observed. In recurrent forms of meibomitis or its chronicity, the formation of a hordeolum—a granuloma of the meibomian gland—may occur.
- Pain and discomfort in the eyelid area.
- Swelling and hyperemia of the conjunctiva.
- Discharge of purulent content from the meibomian gland.
- Characteristic coating on the eyelid.
- Spasms of the eyelid muscles, itching, burning sensation, and redness of the skin.
The specialists’ view on meibomitis therapy
Expert medical opinion on the treatment of meibomitis emphasizes the importance of a comprehensive approach, including both conservative methods and procedures aimed at eliminating factors that contribute to the onset of the disease. One of the main principles of therapy is the drainage of infected meibomian glands, which helps reduce inflammation and promote the rapid recovery of the patient.
Experts recommend the use of topical antimicrobial agents for the treatment of meibomitis, such as antibiotics or sulfonamide-based medications, to reduce bacterial load and prevent complications. Additionally, in some cases, surgical intervention may be necessary to remove a meibomian gland granuloma or improve the drainage of secretions.

Methods for detecting meibomitis
Diagnosis of meibomitis includes a visual examination of the eyelids and eyes to identify signs of inflammation or discharge of purulent material from the meibomian gland. Additionally, palpation of the eyelid is performed to assess tenderness and swelling of the tissues. To confirm the diagnosis, secretion removal from the meibomian gland may be used for laboratory analysis, for example, to identify pathogens.
In cases where the diagnosis of meibomitis is challenging or raises doubts, a referral to a specialist—an ophthalmologist or another physician specializing in eye and eyelid diseases—may be necessary. Such a professional will be able to conduct a more detailed examination, including biomicroscopy, to accurately determine the condition of the meibomian glands and prescribe appropriate treatment.
- Visual examination: the doctor conducts a visual assessment of the eyelids and eyes for signs of inflammation and purulent discharge from the meibomian gland.
- Palpation of the eyelid: a procedure that allows evaluating tenderness and swelling of the eyelid tissues when meibomitis is suspected.
- Extraction of secretions from the meibomian gland: may be used for laboratory analysis, including identifying possible pathogens or causes of inflammation.
- Methods of biomicroscopy: provide the opportunity for a more detailed examination of the meibomian glands and surrounding tissues for accurate diagnosis of meibomitis.
- Consultation with a specialist: if necessary, the doctor may refer to an ophthalmologist for further studies and accurate determination of the diagnosis of meibomitis.
Principles of meibomian gland dysfunction therapy
In cases of severe or recurrent meibomitis, surgical intervention may be required. Procedures such as incision of the meibomian duct (meibomectomy) may be used to remove purulent accumulations and improve the drainage of secretions from the glands, which aids in recovery and prevents recurrence of the disease.
- Application of heat compresses: thermal procedures help to expand meibomian glands, improve blood supply, and facilitate the flow of secretions, reducing inflammation.
- Use of antibiotics: local application of antibiotics helps to fight infection in meibomian glands and prevent its spread.
- Hygienic procedures: an important part of the therapy for meibomitis is maintaining eyelid and eye hygiene, as well as gentle massaging of the eyelids to improve secretion drainage.
- Surgical intervention: in cases of complicated meibomitis, a meibomectomy may be required – a surgery to incise the meibomian ducts to remove purulent accumulations.
- Following specialist recommendations: it is important to consult with a doctor for an individualized treatment plan for meibomitis and to prevent possible complications.
Measures to prevent meibomitis
In order to reduce the risk of developing meibomitis, it is recommended to avoid overheating or overcooling the eyes, as this can lead to a disruption of the functions of the meibomian glands. It is also important to carry out regular hygiene procedures using gentle eyelid care products to avoid clogging the meibomian gland ducts and to reduce the risk of inflammation.
- Eye hygiene: daily washing of the face and cleaning of the eyelids help reduce the risk of meibomian gland infection.
- Avoiding contact with dirty surfaces: preventing the transfer of bacteria to the eyelids can help prevent infection in the meibomian glands.
- Cautious use of cosmetics: choosing quality skincare products for the eyelids and delicately applying makeup contributes to maintaining the health of the meibomian glands.
- Preventing cooling or overheating of the eyes: maintaining an optimal temperature in the environment for the eyes can help preserve normal function of the meibomian glands.
- Regular visits to an ophthalmologist: timely preventive examinations by a specialist help identify potential eyelid problems before they escalate.
Amazing aspects of meibomian glands
An interesting aspect of meibomitis is its impact on the patient’s quality of life due to symptoms such as pain, itching, eyelid swelling, and discomfort. Late or incorrectly diagnosed meibomitis can lead to complications such as chalazion, highlighting the importance of timely medical consultation and adherence to prescribed treatment.