Testicular cancer: diagnosis, treatment, and prognosis
- Understanding Testicular Cancer
- Risk factors for testicular cancer
- The main signs of testicular cancer
- Expert opinion on the treatment of testicular cancer
- Methods for diagnosing Testicular Cancer
- Methods of treating testicular cancer
- Prevention measures for testicular cancer
- Interesting aspects about testicular cancer
- FAQ
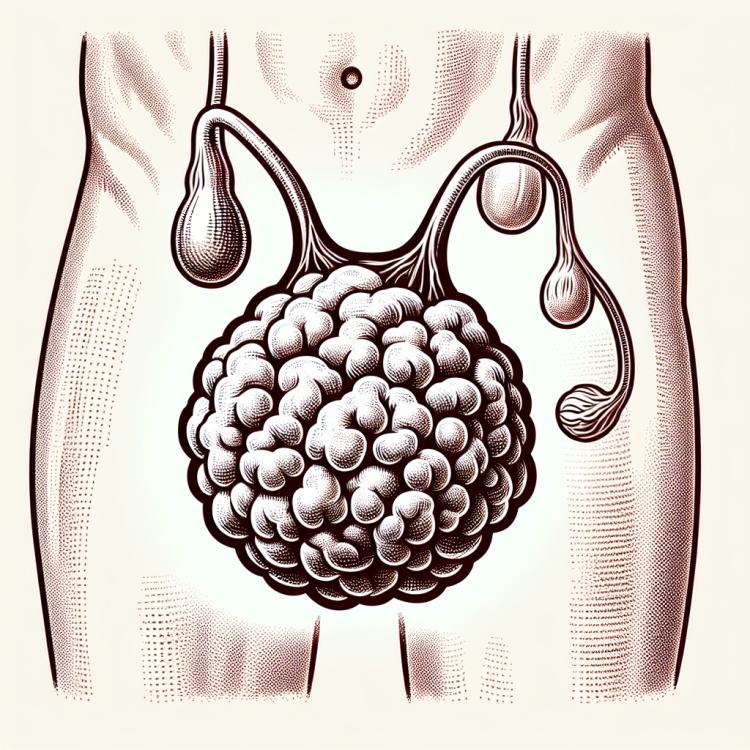
Understanding Testicular Cancer
Testicular cancer is a malignant tumor that arises from the cells of the testicle. This tumor can manifest various symptoms, such as an increase in the size of the testicle, pain, fluid drainage into the scrotum, or changes in the structure of the testicle. Diagnosis of testicular cancer includes physical examination, ultrasound examination, biopsy, and other methods that allow for accurate diagnosis and staging of the disease. Treatment of testicular cancer may involve surgical removal of the tumor, chemotherapy, radiation therapy, or a combination of these, depending on the stage of the disease and the individual characteristics of the patient.
Risk factors for testicular cancer
The exact causes of testicular cancer are not fully established, but there are known risk factors, including genetic predisposition, cryptorchidism (undescended testicles), previous cases of malignant testicular tumors, as well as environmental and medication-related factors. Genetic anomalies, especially Hopkins syndrome, Teaching syndrome, and a family history of testicular cancer, increase the risk of developing this disease. Understanding and identifying these factors help in the diagnosis, prevention, and treatment of testicular cancer and improve the chances of early detection and successful treatment.
- Genetic predisposition: The presence of certain genetic mutations, such as Hopkins syndrome, may increase the risk of testicular cancer.
- Cryptorchidism: Undescended testicles in infancy or childhood is a risk factor for the development of testicular cancer in the future.
- Previous cases of testicular cancer: Having a family history of testicular cancer may increase the likelihood of developing this disease.
- Environmental exposure: Exposure to toxins and chemicals, such as tobacco smoke or radiation, may elevate the risk of testicular cancer.
- Medications factors: Some medications, particularly anabolic steroids, may increase the likelihood of developing testicular cancer.
The main signs of testicular cancer
The main signs of testicular cancer may include enlargement or hardening of the testicle, increased or constant dull aching sensation in the scrotum, swelling of the testicle, as well as the discovery of a lump or nodules during self-examination of the testicle. Some patients may also experience swelling or a feeling of heaviness in the scrotal area, pain or discomfort in the abdomen or lower back. As the disease progresses, symptoms may intensify, and there may be signs of metastasis, such as pain during urination, swelling in the urinary tract area, bleeding, or pain while breathing, which requires immediate medical attention for diagnosis and treatment.
- Thickening or enlargement of the testicle: Patients usually notice changes in the structure or size of the testicle during self-examination.
- Frequent or constant aching sensation in the scrotum: The appearance of pain, especially if persistent or increasing over time, may be a sign of testicular cancer.
- Swelling of the testicle: An increase in the size of the testicle due to fluid retention can be one of the symptoms of testicular cancer.
- Thickening or lumps during self-examination: Finding unusual thickening or lumps during examination of the testicle may also indicate a problem.
- Swelling or feeling of heaviness in the scrotum: Unusual sensations in the scrotal area, such as swelling or a feeling of pressure, can be a sign of testicular cancer.
Expert opinion on the treatment of testicular cancer
Expert opinions on the treatment of testicular cancer are based on a comprehensive approach tailored to each patient. Oncology experts emphasize the importance of early detection and a differentiated approach to selecting treatment methods depending on the stage of the disease. Surgical intervention to remove the tumor is one of the main therapeutic methods and is often accompanied by chemotherapy or radiation therapy for more effective control of the growth and spread of cancer cells.
Experts also highlight the importance of psychological support for patients during the treatment process for testicular cancer, as the disease can have a significant psycho-emotional impact on the patient. Close interaction among medical professionals of various specialties allows for optimal treatment, reducing the risk of recurrence and improving the prognosis for each specific patient.

Methods for diagnosing Testicular Cancer
The diagnosis of testicular cancer includes a number of methods, such as a physical examination to determine enlargement or hardening of the testicle, ultrasound to visualize changes in the testicles, blood tests to identify specific tumor markers such as alpha-fetoprotein and beta-human chorionic gonadotropin, and computed tomography to confirm the presence of a tumor and assess its extent. Additional methods, such as magnetic resonance imaging (MRI) and biopsy, may be applied to clarify the diagnosis and plan treatment. It is important to consult a doctor in a timely manner when suspicious signs arise to begin diagnosis and treatment in the early stages of the disease.
- Physical examination: the doctor conducts an inspection and palpation to identify changes in the testicles.
- Ultrasound examination: allows visualization of the tissues of the testicles and detection of tumors or other pathologies.
- Blood tests for tumor markers: measurement of levels of alpha-fetoprotein (AFP) and beta-human chorionic gonadotropin (β-hCG) to assess cancer processes in the testicles.
- Computed tomography (CT): helps determine the extent of the tumor and identify metastases in other organs.
- Magnetic resonance imaging (MRI): provides additional information about the structure and condition of the testicular tissues for accurate diagnosis of testicular cancer.
Methods of treating testicular cancer
- Surgical intervention: The basis of the treatment strategy for testicular cancer often lies in orchiectomy, the surgery to remove one or both testicles, including surrounding tissues, to prevent the spread of cancer cells.
- Chemotherapy: Used to destroy cancer cells, often after surgery, or in cases of metastasis. Chemotherapy can be conducted as mono- or combination therapy.
- Radiotherapy: Used for radiation exposure to the tumor and can be applied before surgery to reduce the size of the tumor or after to treat residual cells and reduce the risk of recurrence.
- Monitoring tumor markers: Certain proteins in the blood can serve as indicators of treatment effectiveness and the presence of recurrence. Regular monitoring of markers helps in assessing the patient’s condition.
- Targeted drugs and immunotherapy: New approaches to treating testicular cancer include the use of drugs that target specific molecular targets in the tumor, as well as using immune mechanisms to combat cancer cells.
Prevention measures for testicular cancer
- Regular self-examination: it is important to conduct regular self-examinations of the testicles to detect any enlargement or pathological changes.
- Regular doctor visits: it is recommended to see a doctor for preventive check-ups and monitoring of testicular health.
- Maintaining a healthy lifestyle: moderate physical activity and a healthy diet contribute to overall health and reduce the risk of testicular cancer.
- Adhering to preventive measures for those at increased risk: special attention should be given to individuals with a genetic predisposition or risks such as cryptorchidism.
- Early detection and prevention of risk factors: key measures remain the early detection and prevention of risk factors for developing testicular cancer.